– Edgar Rodney Buregeya
As we mark World Day of Social Justice, Uganda finds itself at a defining moment. This year’s theme, Empowering Inclusion: Bridging the Gaps for Social Justice, challenges us to examine whether the rights guaranteed in our Constitution are reflected in people’s daily lives, especially in a period shaped by political transition and socio-economic strain that continue to weigh heavily on the most vulnerable.
The recent parliamentary elections signal this shift. Only 40 percent of Members of Parliament were re-elected. The remaining 60 percent include legislators who championed social justice causes. Whether that legacy endures will depend on how firmly these issues remain anchored in national priorities.
Social justice is not abstract. It is the difference between a mother who accesses emergency obstetric care and one of the 12 women in Uganda who dies from preventable pregnancy-related complications, according to estimates from the Uganda Bureau of Statistics. At its core, social justice addresses the structural conditions that reproduce inequality: underfunded health systems, unsafe environments, and livelihoods stripped of dignity.
Uganda’s Constitution guarantees fundamental rights, and successive National Development Plans have committed to Universal Health Coverage and equitable service delivery. Yet the gaps are stark. Eighty-two districts operate without a general hospital. Many sub-counties lack a functional Health Centre III. More than half of Uganda’s youth are neither employed nor in education or training. Over seven million Ugandans, about 16.1 percent of the population, live below the national poverty line. These are not isolated statistics; they reflect systemic inequities.
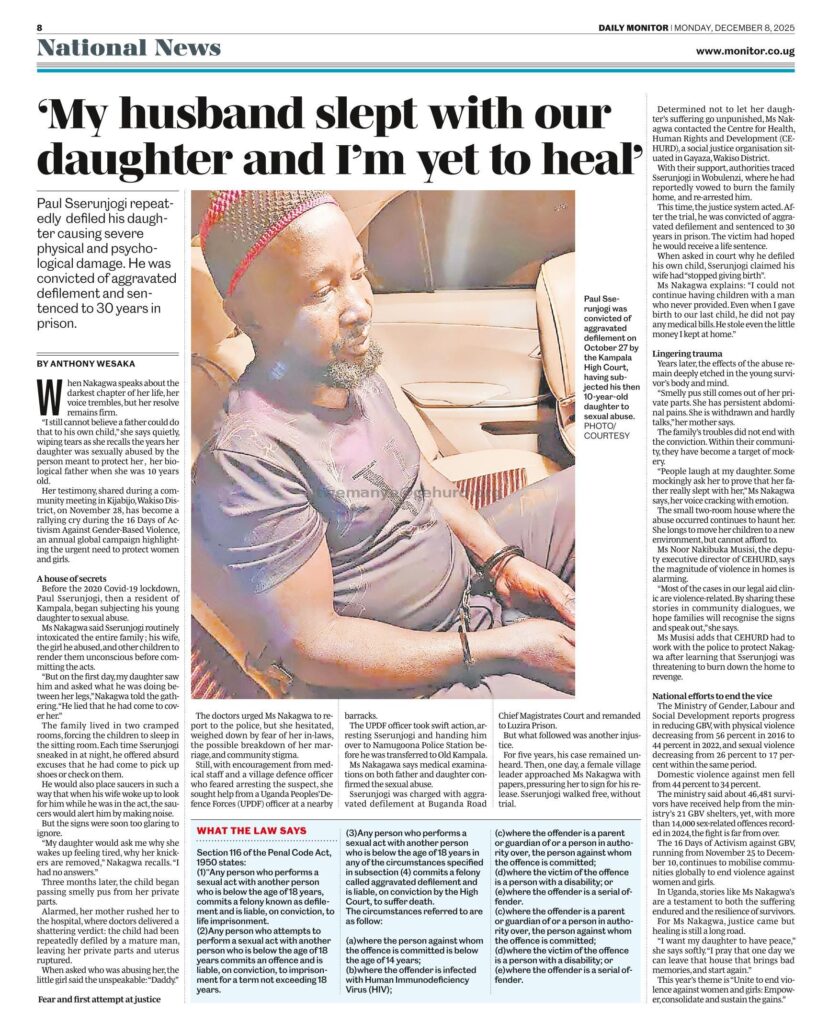
For sixteen years, the Center for Health, Human Rights and Development (CEHURD), alongside other advocates, has worked to close these gaps through litigation, research, policy advocacy, and community empowerment. Our experience shows that change becomes possible when institutions are held accountable and communities understand and assert their rights.
In 2024, CEHURD secured a landmark judgment from the High Court holding Mulago National Referral Hospital liable for the disappearance of a newborn. The Court affirmed not only the right to health, but also the State’s obligation to provide psychosocial support to victims of health rights violations. Accountability, the Court made clear, is central to justice.
In May 2025, CEHURD filed a civil suit against the Kampala Capital City Authority and the National Environment Management Authority following the catastrophic collapse of the Kiteezi landfill. The disaster claimed lives and destroyed homes after prolonged warnings about hazardous waste leakage and environmental risk. The Kiteezi community, largely low-income, had long been exposed to preventable harm. The case seeks more than compensation. It calls for systemic reform, safe decommissioning of hazardous infrastructure, environmental restoration, and sustainable waste management that prioritises community health.
Beyond the courts, CEHURD has supported the development and implementation of Uganda’s National Guideline on Self-Care Interventions. This framework strengthens individuals’ ability to manage aspects of their reproductive, physical, mental, and emotional well-being. Through collaboration with the Ministry of Health and grassroots engagement, this work has advanced outcomes in sexual and reproductive health and rights, gender justice, communicable and non-communicable diseases, and mental health.
In September 2025, CEHURD convened the second Uganda National Conference on Health, Human Rights and Development, culminating in the Uganda Declaration on Social Determinants of Health. The declaration recognises a simple truth: most health outcomes are shaped outside hospital walls. Housing, education, environment, nutrition, and gender equality are not peripheral concerns. They determine who lives well and who does not.
World Day of Social Justice in 2026 should therefore serve as a benchmark for policy action. While the National Development Plan IV outlines ambitious commitments, implementation must be matched with equitable financing, functional infrastructure, and measurable accountability.
The Government of Uganda must operationalise the right to health through legislation, budgeting, and coordinated action across ministries including Education and Sports; Water and Environment; Justice and Constitutional Affairs; and Gender, Labour and Social Development. Environmental negligence must carry consequences. Independent oversight mechanisms are essential to prevent tragedies such as Kiteezi from recurring.
This also requires a civic space where public interest advocacy can function without undue restriction. When civil society and communities are constrained, accountability weakens and development outcomes suffer.
Advancing social justice is a shared responsibility. Government carries primary constitutional duties, but meaningful progress depends on cooperation among institutions, communities, and citizens. The promise is a Uganda where a newborn’s survival does not depend on geography or family income, where communities breathe clean air and drink safe water, and where health systems serve all with dignity.
The measure of this commemoration will not be speeches delivered, but structural gaps closed. Health justice and social justice are inseparable. Both demand sustained commitment, principled leadership, and collective accountability.
The writer is a Legal Clerk at the Center for Health, Human Rights and Development (CEHURD).