Synergistically cultivate client-centered experiences without cross-media initiatives. Dynamically develop 2.0 web services with top-line partnerships. Phosfluorescently maintain inexpensive alignments before virtual infomediaries. Seamlessly pontificate cost effective data vis-a-vis pandemic opportunities. Professionally productize quality e-commerce rather than client-centric infomediaries. Read More PROFESSIONAL PORTALS
Synergistically cultivate client-centered experiences without cross-media initiatives. Dynamically develop 2.0 web services with top-line partnerships. Phosfluorescently maintain inexpensive alignments before virtual infomediaries. Seamlessly pontificate cost effective data vis-a-vis pandemic opportunities. Professionally productize quality e-commerce rather than client-centric infomediaries. Read More OFFICIA DESERUNT
Only one thing is impossible for God: To find any sense in any copyright law on the planet. Mark Twain
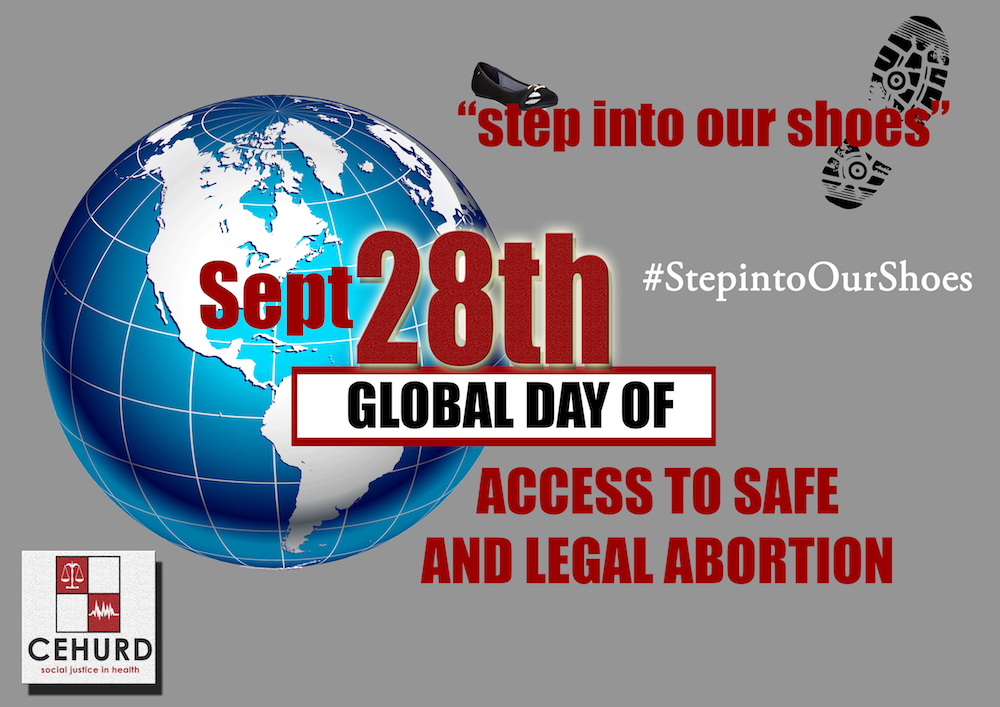
Global Day of Access to Safe and Legal Abortion: take a minute to think of the appalling statistics on abortion in Uganda
As we join the rest of the world to mark the Global Day of Access to Safe and Legal Abortion under the theme:Stepping into Our Shoes, take a minute to think of the appalling statistics on abortion in Uganda.
In Uganda, over 300,000 abortions occur annually , and the vast majority of these are unsafe. Of the 6,000 deaths annually of women due to pregnancy or childbirth , 1200 women will die from unsafe abortion, and further 85,000 women will be treated for complications of abortion.
The estimated rate of 54 abortions per 1000 women of reproductive age is far higher than the East African average of 36 abortions per 1,000. Currently approximately 40% of admissions for emergency obstetric care in Uganda are a result of unsafe abortion.
The Center for Health Human Rights and Development (CEHURD) is dedicated to work towards achieving access to safe and legal abortion in Uganda.

Information session for Persons Living with HIV and sex workers in Buikwe district
The fishing communities of Kiyindi Landing site in Buikwe District had the opportunity to have an information session on prevention, treatment mechanisms of HIV/AIDS and TB and reduction of stigma and discrimination at the community level organised by CEHURD. The targeted groups included Persons Living with HIV, sex works, Community Health Advocates in the areas of Najja and Nyenga.
Dr. Grace Mugabi an HIV / TB specialist at the session said that Buikwe district has a high HIV prevalence than other parts of the country and advised that individuals should test for HIV every after three months because of the widal period where the virus may not be detected in the human body.
He talked to participants about the treatment target to help end the AIDS epidemic called the 90%-90%-90%, that sets out to ensure that by 2020, 90% of all people living with HIV will know their HIV status. By 2020, 90% of all people with diagnosed HIV infection will receive sustained antiretroviral therapy and that by 2020, 90% of all people receiving antiretroviral therapy will have viral suppression.
He further stated that to achieve the 90%, 90%,90% plan there should be no stigma against the people with HIV increased involvement of mothers should be paramount and so should of male involvement.
On the concern of stigma and discrimination of PLHIV, participants said that in their communities name calling is seen as a common practise names like “kasilimu” have been used by community members to refer to some of the PLHIVs. This they say they have become used to but agreed is wrong and something needs to be done about it.
Recommendations made by Persons Living with HIV and the sex workers included;
- An anti-stigma and discrimination policy should be put in place to protect those with HIV from any form of unfair treatment in society.
- HIV positive children in schools should be given an opportunity to take their ARVs at the right time.
- Prisoners should also be given an opportunity to take their ARVs at the right time.
- More community outreaches are needed to ensure that people are taught how to welcome those with HIV back in the community and ensure that they are supported and looked after.
At the end of the information session participants who included PLHIV, sex workers, and community health advocates who said they had acquired information about stigma and discrimination, the session also taught them to keep a close watch to their children and talk to them about HIV and lastly it gave them strength to openly talk about HIV and their statuses.
Cissy Nagita one of the beneficiaries from the information session said, ” the training has given me strength to do more outreaches to get more people in my community on board in the fight against HIV, stigma and discrimination.”
