By Edith Sifuna
Sophia (not real name) could not easily access transport to the nearby health centre for maternal services. She therefore resorted to seeking the services of a traditional birth attendant (TBA) in a neighbouring village. She could not trek the long distance to deliver her child since she had gone into labour late in the night while she was home alone. An elderly TBA was her only option to deliver the baby. Unfortunately, Sophia suffered from obstructed labour and by the time she accessed a boda boda to get to the health care facility, she had lost her baby and had passed out. The midwife on duty could only give her first aid as they waited for an ambulance from the nearby private hospital to take her for further treatment.
With the global outbreak of COVID-19, Uganda took steps to curb the spread of the virus. Some of these steps included the Presidential directives that put restrictions on movement. These restrictions included a ban on public and private transport, except for essential services. Sophia is one of the many expectant women in Uganda who have been reported to resort to TBAs to give birth from villages due to these restrictions. Women have lost their lives while giving birth, lost their babies and or left the labour ward with complications and other psycho-social effects. COVID-19 like many other pandemics attacked Uganda unprepared more so because of the need to strike a balance between control of the pandemic and provision of essential health services where maternal and child health have been at the peak.
Uganda’s maternal mortality ratio stands at 336 deaths per 100,000 live births according to the Uganda Demographic and Health Survey 2016, with an average of 16 women dying daily while giving birth due to preventable causes. This figure is less likely to reduce to the projected indicators in the Sustainable Development Goals (SDGs). Even if the State worked hard to achieve the set indicators, the effects of the COVID-19 pandemic already show a failure to achieve them. As part of ensuring that this pandemic is suppressed, the President of the Republic of Uganda working with the COVID-19 task force in the Ministry of Health provided directives to the country that were welcomed at the time. The country was in fear and everyone thought that these were indeed great directives. Reality, however, set in when expectant mothers continued to die and others delivered by the roadside or at the entrance of facilities due to movement restrictions.
The restriction on movement affected both women due for delivery and those due for antenatal care (ANC) visits. The World Health Organisation Guidelines (WHO), set at least eight antenatal care visits from the initial four as a measure for monitoring the well being of the expectant mother and the unborn
baby. These are unfortunately not possible for most expectant women due to the COVID-19 restrictions.
Many expectant women have instead been reported to have faced police brutalities while trying to access the health facilities. For example a video recording circulated on May 8th, 2020 showing a Local Defence Unit (LDU) officer shooting a boda boda rider and an expectant woman who were on their way to the hospital in Masaka. Both were reported dead. This happened despite the President relaxing restrictions on the movement of pregnant women on boda bodas.
Women have also failed to access necessary health care due to the economic breakdown brought about by COVID. Many have lost jobs and cannot earn a living. Additionally, movement restrictions especially in regard to public transport have caused a hike in transport fares, which many find too high to enable them access services. The current curfew which stops movement at 7pm has not made things easier.
These conditions, among others, have left expectant women with few options. The TBAs became the silent saviours of women’s lives. These were willing and ready to accord the much needed timely support for the expectant mothers in their communities for a number of reasons. First, they live within the communities and are therefore not affected by the movement restrictions. Secondly, the support and care TBAs accord women while they are in labour is sometimes not equivalent to the one provided in health facilities because the numbers attended to at a time is smaller.
It should be noted that in 2010, the Government of Uganda outlawed TBAs. They were banned from conducting deliveries as they lack formal training to handle emergency cases such as C-Sections and haemorrhage. Haemorrhage contributes to 46 per cent of maternal mortality among women according to the 2018/2018 Maternal Perinatal Death Survey Report (MPDSR). Despite the ban, the traditional birth attendants are still very active, providing maternity care during and after pregnancy, especially in rural communities. Expectant mothers’ preference to traditional birth attendants’ services has risen even higher during the COVID-19 period. Beyond proximity, the current socio-economic and mobility challenges have seen women run to TBAs even more. Unfortunately, the delivery places and services are of very poor quality and usually take place under unhygienic conditions with no referral systems.
Most TBAs in villages are old and have no training to offer timely technical assistance to expectant mothers but because they command a lot of respect, most people respect them and have resorted to their services.
The outbreak of the pandemic saw the designation of some facilities to handle COVID-19 cases. This meant that attention to general sexual and reproductive health and rights services including maternal health services was minimised. Managing COVID-19 remains Uganda’s priority. Furthermore, there are myths and misconceptions about the behaviour of healthcare providers as being harsh and rude, although they have been found to be this way, especially towards expectant mothers. On the other hand, TBAs are perceived as approachable, friendly and are known to deal well with financially constrained mothers as they sometimes go to the extent of giving them tea and food in addition to some herbal concoctions. These factors therefore make TBAs more attractive to expectant women in the communities. However, the services of TBAs have been known to increase maternal mortality, mother to child transmission of HIV/AIDS (MTCT) and postpartum haemorrhage. These indicators are expected to worsen if mothers continue giving birth with the assistance of TBAs who are not equipped to handle such emergencies and cannot easily refer the women to health facilities where they can be skillfully helped.
The presidential directives were put in place to protect Ugandans from COVID-19 and curb its spread in communities. However, the country has registered more maternal deaths than COVID-19 ones, which still stand at zero, due to the inability to access transport to health facilities. As CEHURD, we therefore recommend that the Ministry of Health strengthens the Public- Private Partnership (PPP) in this era to extend quality, accessible and affordable health services to all places in the country but more so to rural communities.
This can be done through working with different civil society organisations and other private actors to provide services and information to the masses. These collaborations are also an avenue to advocate for better service delivery and accountability. They also contribute to strengthening the local community structures such as Village Health Teams (VHTs), Health Unit Management Committees (HUMCs), and Community Health Advocates (CHAs).
VHTs if extensively trained and given the skills training, can take record of all expectant mothers in their constituencies and constantly monitor them till delivery time. They can further support them to access health facilities for ANC and child delivery, not forgetting social distancing and personal protection with protective gear, constant hand washing and use of alcohol-based sanitisers. They can also offer health education to their constituencies.
HUMCs can be further strengthened to continuously update the communities about the available services at facilities and encourage them to go for health care. They can further monitor the activities of the health workers and quality of services. However, health workers should be equipped with the adequate personal protective gear such as emergency drugs, gloves, masks and disinfectants, among others as they are also working in fear of their safety while dealing with different categories of people from diverse locations.
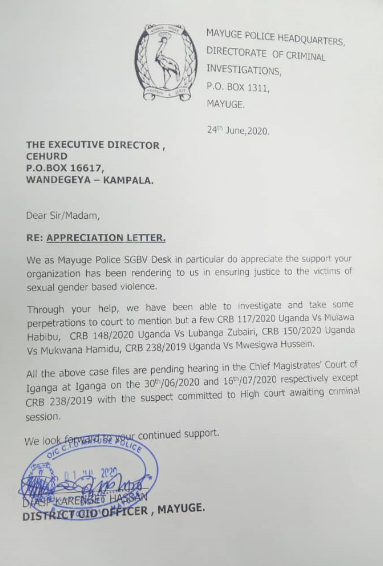
Lastly, Center for Health, Human Rights and Development (CEHURD) has trained a team of Community Health Advocates (CHAs) who are advocating for the realisation of right to health within communities. They also report cases such as Sophia’s. CHAs can sensitise communities about their rights and responsibilities amid COVID-19, record and report health rights violations and refer those who may need legal aid to CEHURD through the toll free line – 0800 31 3131. All this should be done in respect to MOH guidelines.
The right to health is inherent and ought to be protected especially the lives of mothers and their newborn babies. Health workers should be supported to save lives and mothers taken good care of while bringing life to earth. Despite the pandemic, reproductive and maternal functions are ongoing, even escalated by the lock down, characterised by high sexual engagement both consensual and non-consensual. COVID-19 is a big public health threat but not worse than maternal deaths, this is evidenced by the fact that mothers and babies have been and are continuing to be lost due to effects of the lock down. Under these circumstances, isn’t it time for the country to re-think its restrictions and prioritise access to quality maternal and child health services? It’s unacceptable for women to die at the hands of traditional birth attendants and COVID-19 should be a learning opportunity for the Ugandan government. At the moment, Uganda is exposed and we need to work harder to ensure that women’s lives are protected and not lose another woman due to preventable child-birth related complications.
For God and my Country.
The writer is a programme officer at Center for Health, Human Rights and Development (CEHURD).
A version of this article was originally published in the Daily Monitor on 11th July 2020.